By Bill Thomas | April 1, 2024
From leukemias and lymphomas to carcinomas and sarcomas, there are many, many different types of cancer, and no two are identical. Just as there are major differences between brain cancer and blood cancer, so too is there a world of difference between cancers in children and cancers in adults.
Here at the Pediatric Cancer Research Foundation, we’ve made it our mission to help advance pediatric cancer research so that, someday, no child will have to perish due to cancer or cancer-related complications. Our vision is of a world where every form of childhood cancer has a cure. Before we can make that vision a reality, though, we believe it’s important to acknowledge the unique challenges that pediatric cancer represents.
Here’s what you should know about how pediatric and adult cancers differs.
The Causes of Pediatric Cancers are Different
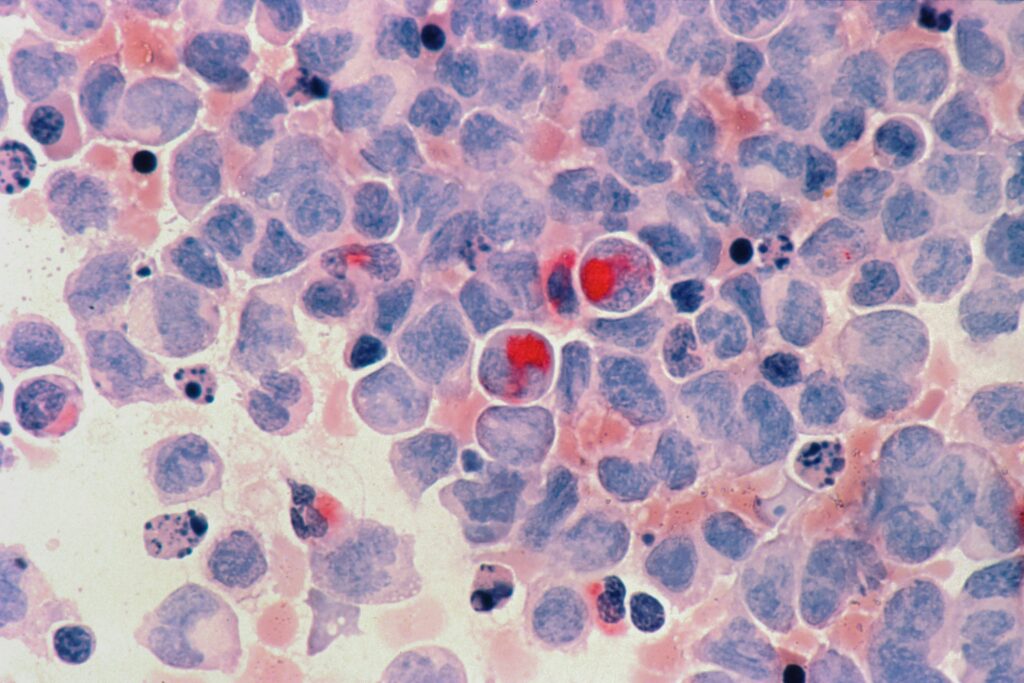
Differences between pediatric and adult cancers begin at the fundamental level. Indeed, they are present in the very biologies of the disparate age groups.
“There is a common misconception that children are just small adults, but this couldn’t be farther from the truth,” Dr. Amanda Saratsis, a pediatric neurosurgeon at Advocate Lutheran General Hospital in Park Ridge, IL and PCRF board member, explains. “The biology of a developing human is distinct from that of a mature adult. Treatment strategies that work for adults often have no effect in pediatric cancers due to their distinct biology.”
Effectively treating a cancer patient, of course, requires understanding the cause of their disease. In the case of adult patients, cancer is typically caused by natural aging, lifestyle choices and/or environmental factors. Decades of exposure to UV rays or cigarette smoke, for example, can result in the accumulation of genetic mutations, which increase one’s risk of cancer over time.
Children can also develop cancers due to carcinogen exposure. However, in many cases, cancer-causing mutations occur in children spontaneously and unpredictably. This poses a challenge during diagnosis, as parents may be less likely to notice or report certain symptoms. That said, the way cancer operates in developing bodies does offer some unique advantages, as well.
“Pediatric cancers are often caused by one or two mutations, whereas adult cancers can be the result of tens or even hundreds of mutations,” Dr. Elliot Stieglitz, a pediatric oncologist at UCSF Benioff Children’s Hospital, says. “This has important implications when thinking about targeted treatment which can typically only address one mutation at a time. Since we can only use one or, at maximum, two targeted medications at a time, this means that pediatric cancers are actually more likely to respond to targeted treatment than adult cancers.”
Outcomes for Pediatric Cancers are Better
Regardless of age, cancer is always a difficult disease, not just for doctors to treat but also for patients to endure. Having said that, it’s worth noting that pediatric cancer patients have higher rates of survivorship than adult patients. The National Institute of Health reports that 69% of all cancer patients have a 5-year survival rate. The 5-year survival rate for children specifically, meanwhile, ranges from 85-87%, depending on age.
Part of this can be attributed to the fact that pediatric cancer patients have fewer non-cancer-related health issues than adult patients. This allows the body’s immune system to better focus on fighting the cancer cells. It also means that pediatric cancer patients are generally more resilient, allowing doctors to consider treatments that may be too much for older patients to handle.
“Children tolerate chemotherapy better than adults because their organs are healthier,” Dr. Kathleen Sakamoto, a professor of pediatric hematology and oncology at Stanford University School of Medicine, says. “Therefore, the approach to treatment of their cancers is often different.”
Additionally, while differences in biology mean that breakthroughs in adult cancer treatment don’t always translate into comparable advances for pediatric patients, pediatric cancer researchers nevertheless benefit from prior research conducted using adult subjects.
“Studies in adults are often ‘first in human.’ This entails a greater risk, which is appropriate considering the poor outcomes in adults,” Dr. Stieglitz says. “Typically, when trials are started in pediatrics, they have already been tested in adults, so a general sense of safety is already established and it is more about finding the ‘correct’ dose for children.”
Long-Term Side Effects are a Major Concern

The better outcomes enjoyed by pediatric cancer patients mean that children who survive a cancer diagnosis generally live longer than adults. Being able to look forward to the future is a gift for cancer patients, but it’s also something their doctors must be mindful of when presenting treatment options.
“Pediatric patients, if cured, have a long life ahead of them,” Cherie Daly, vice president clinical research physician at Nuvation Bio and PCRF’s director of scientific affairs, opined. “Long-term side effects and future quality of life play a critical role in decisions around treatment and treatment goals.”
While doctors always want to improve their patients’ quality of life, long-term side effects are usually a secondary concern when treating older patients. Greater emphasis is often placed on simply prolonging their life and making them as comfortable as possible. Since fewer adult patients live longer than five years following a cancer diagnosis, the likelihood of them experiencing harmful side effects from treatment is minimal.
On the other hand, due to having longer lifespans, childhood cancer survivors are at a greater risk of suffering long-term issues, including hormone dysregulation, lost muscle mass, uneven limb length, hearing loss, brain damage, and infertility. This can make it difficult for doctors to find treatment options that are both safe and effective, and even more difficult for families struggling to make the right decision for their child’s well-being.
For researchers, meanwhile, the importance of preserving quality of life for pediatric cancer patients is a significant motivating factor in how treatment avenues are studied. “Adult cancer research is often about extending the length of time before the cancer eventually returns,” Stieglitz says. “Pediatric cancer trials attempt for cures, not just prolongation in life.”
Cancer is Rarer in Children Than in Adults
According to the National Institute of Health, more than 80% percent of U.S. cancer cases are diagnosed in patients older than 55. Meanwhile, cancer patients under the age of 20 account for just 1% of all cancer diagnoses in the United States.
That may seem like a small number, but even 1% of the 1.9 million people diagnosed with cancer each year is a lot. The NIH estimates that 15,190 children and adolescents were newly diagnosed with cancer in 2023 and that 1,590 pediatric cancer patients died from the disease that year.
With numbers like these, it’s clear that, despite its relative rarity, pediatric cancer is a serious issue. Indeed, pediatric cancer is the leading cause of death by disease among children under 20 in the U.S. Unfortunately, the lower incidence of cancers in children often presents unique obstacles to researchers.
“It is much harder to enroll statistically significant numbers of pediatric patients for a clinical trial compared to the adult population,” Dr. Saratsis says, pointing out how difficult it can be finding enough subjects to support each phase of research. “It makes enrollment in trials harder, collection of specimens for testing and development of preclinical models more difficult and raising public awareness and concern more of a challenge.”
What’s more, the rarity of many types of pediatric cancers means that even patients who could participate in a trial may not always be able to. In some cases, the medical center where a trial is being conducted may be hundreds of miles away from the patient’s home.
“It is extremely difficult for families to move to a different center to access those trials. It may be easier for an adult to pick him or herself up and travel to MD Anderson Cancer Center in Texas, for example, without disrupting the entire family,” Stieglitz says. “I think assisting families with logistics to travel to specialized centers is critical.”
Funding for Research is Often in Short Supply

Enrollment complications aren’t the only way in which pediatric cancer’s relative rarity creates complications for researchers. Arguably the biggest obstacle pediatric cancer research needs to overcome is the limited amount of funding currently available. Philanthropic organizations like the Pediatric Cancer Research Foundation are able to help support innovative research projects thanks to the generosity of our donors. Even then, we can only do so much. Last year, due to our own funding scarcity, the Foundation was only able to fund 3.8 percent of grant requests rated outstanding.
“Pediatric cancers are rare, so they don’t get as much funding from Big Pharma, biotech companies, or the government,” Dr. Daly says. “The FDA has implemented regulations with regards to pediatric study plans, but this has not made the impact necessary to move the needle for pediatric cancer research funding.”
To illustrate just how little funding is available for pediatric cancer research, consider that the largest single funding resource, the federal government, invests just 4 cents of every cancer research dollar into childhood cancer. Pharmaceutical and biotech companies are often even more reluctant to invest. Why? Because pediatric cancer treatments are not that profitable.
“There are fewer industry-sponsored clinical trials and fewer available therapies from drug companies for pediatric oncology patients. Because the pediatric oncology market is small, pharmaceutical companies don’t invest in the development of drugs for pediatric cancers,” Dr. Sakamoto explained. “Companies do not want to take the risk or invest in developing drugs for such a small market.”
Although the difficulties facing pediatric cancer researchers are significant, progress is still being made. Over the years, breakthroughs funded by the Pediatric Cancer Research Foundation have helped drive pediatric cancer research forward, developing newer, better treatment options for the patients who need them most. There’s a lot more work to be done, however. There are still childhood cancers that have no cures; and others that need to be improved to be less toxic. If you would like to help us continue supporting life-saving pediatric cancer research, please consider making a donation today.
Additionally, make sure to follow our Profectus blog to stay up to date on all the latest news in pediatric cancer research!