By Bill Thomas | October 2, 2023
Why do some cancer cells not respond to treatment at all? And why do tumors that were initially responsive to therapy eventually become resistant to further treatment? These are among the pivotal questions that will be explored in the treatment of Rhabdomyosarcoma (RMS), a rare but aggressive pediatric cancer of the muscle, thanks in part to a major gift by Heather and Josh Johnston. The couple is supporting research being conducted by Dr. Kyle MacQuarrie at Lurie Children’s Hospital in Chicago.
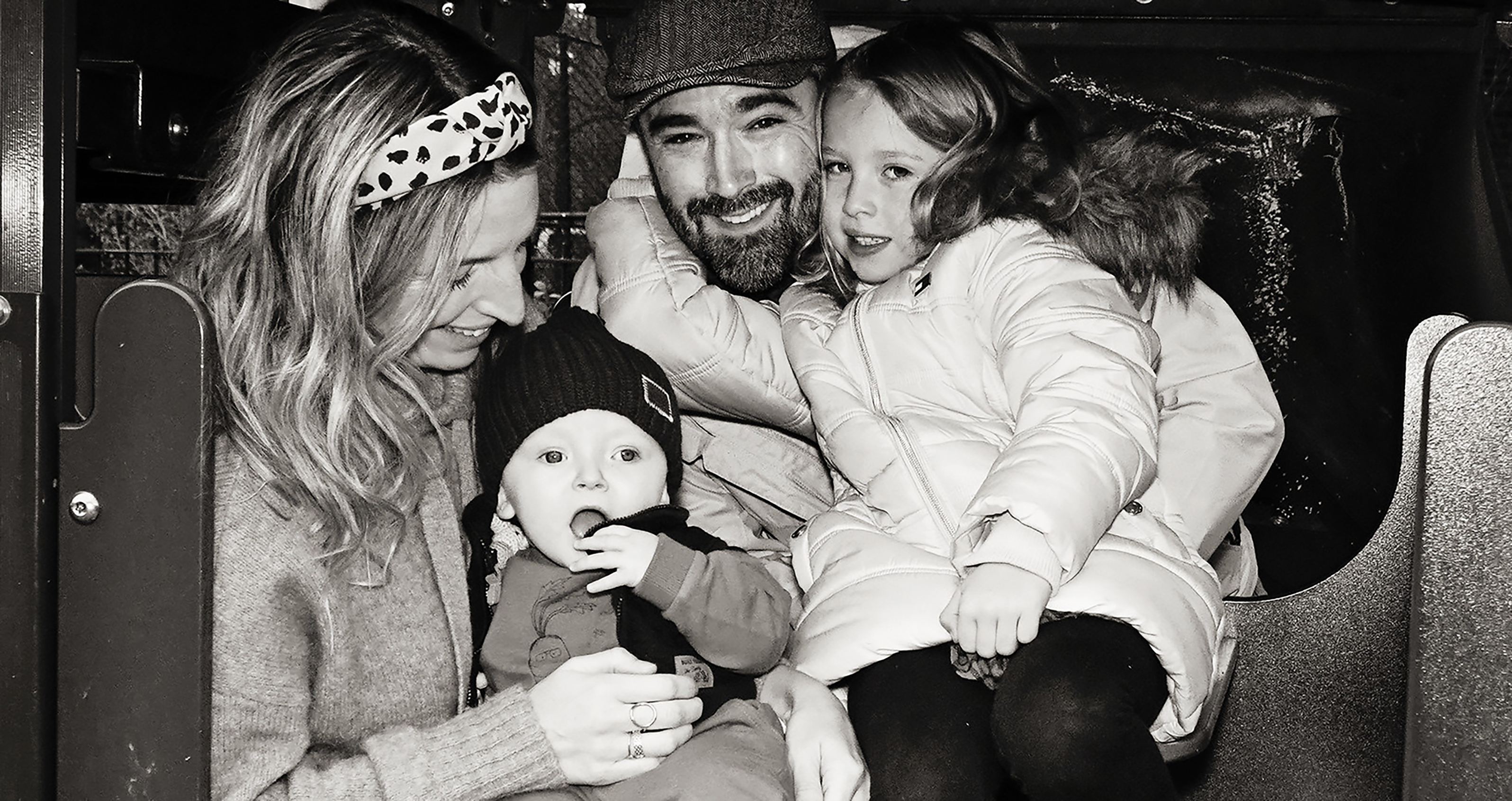
The Johnstons are intimately familiar with the need for accelerating knowledge into Rhabdomyosarcoma and are driven to change the status quo. In 2021, their newborn son, Asher, was diagnosed with stage 1 Alveolar Rhabdomyosarcoma. When he was just four months old, the couple learned that the disease had metastasized throughout his central nervous system with no viable treatment options that would yield positive outcomes. Ever since, Heather and Josh have honored Asher’s brief life by funding research that yields new insights into this ravaging disease.
“Our four-month-old was given a 20-year-old
chemotherapy regimen using drugs developed for
full-grown adults.”
“Rhabdo is among the rarest of pediatric cancers and there has been limited research into it. Our four-month-old was given a 20-year-old chemotherapy regimen using drugs developed for full-grown adults. We are happy to provide financial resources so more knowledge can be gained about treating Rhabdo,” Josh Johnston said.

About 350 American children, teens and young adults are diagnosed with Rhabdomyosarcoma each year. It can arise in nearly any part of the body and is treated with intensive chemotherapy, plus “local control therapy” which includes surgical removal of the masses, radiation therapy to the masses, or both. Many patients initially experience dramatic responses to therapy and some patients are cured. For other patients, the cancer returns during therapy or after completion of therapy. Once patients experience a relapse, curing them of RMS becomes much more difficult.
In more common cancer types, studies have shown that treatment resistance is caused by changes in the tumor cells – what is called tumor evolution – especially through the acquisition of new mutations that make cancer cells resistant to chemotherapy or other treatments.

Dr. MacQuarrie’s research looks at how the organization within the cells affects tumor resistance to chemotherapy. While many studies of chemotherapy resistance in Rhabdomyosarcoma have focused on individual factors and their impact, Dr. MacQuarrie’s work will focus on the changes that occur in the organization over time, not just the individual factors (like individual genes). He hopes understanding the organization will identify new ways to make resistant tumor cells sensitive to chemotherapy and improve treatment of children with tumors that recur or are resistant to treatment when they first occur.
This research project builds upon Dr. MacQuarrie’s 16 years of study into the biology of Rhabdomyosarcoma. As he explains, “Rhabdomyosarcoma tumors sometimes possess a ‘fusion’ between two genes that leads to poor survival. I believe the fusion affects the way the parts of the cell nucleus – the control center of the cell – are organized and that parts of the nucleus that change their organization in normal skeletal muscle cells fail to make these changes in Rhabdomyosarcomas. These organizational changes may help explain why gene fusions occur in these cells. By understanding the differences in organization that are present between the tumor cells and normal cells, and how that relates to cell function, I hope we can understand the origin of these fusions.”
“It is our fervent wish that this research will result
in the addition of new treatments that will
improve cure rates for this life-shattering disease.”
~ Heather Johnston