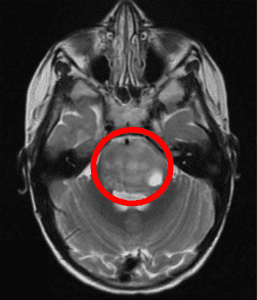
Advances in the diagnosis and treatment of patients with pediatric brain tumors have enabled many to live longer with better cognitive outcomes. In the case of diffuse intrinsic pontine glioma, or DIPG, this is not the case (Figure 1). Children with this form of brain tumor, which arises deep within the brainstem and cannot be removed with surgery, often survive only 9-12 months from their diagnosis, making DIPG the most deadly pediatric cancer. Despite researchers working for over 45 years to improve our understanding of the molecular biology of this disease and testing novel therapies for DIPG, there has been no change in overall survival in these patients. One of the reasons for this is that it is very difficult to get the necessary dose of chemotherapy drug into the tumor, due to what is known as the blood-brain-barrier, or BBB. The BBB is maintained by the endothelial cells that line the blood vessels in the brain to protect the brain from harmful substances that may be in the circulation. Unfortunately, most chemotherapy drugs are too large to cross the BBB, making effective drug delivery to the tumor very challenging.
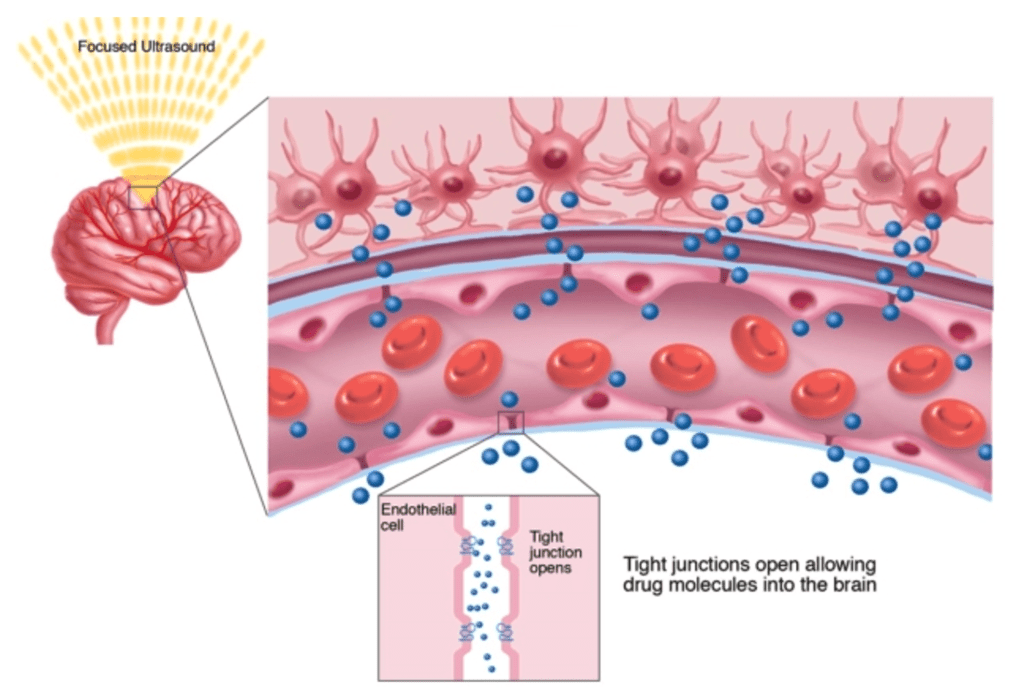
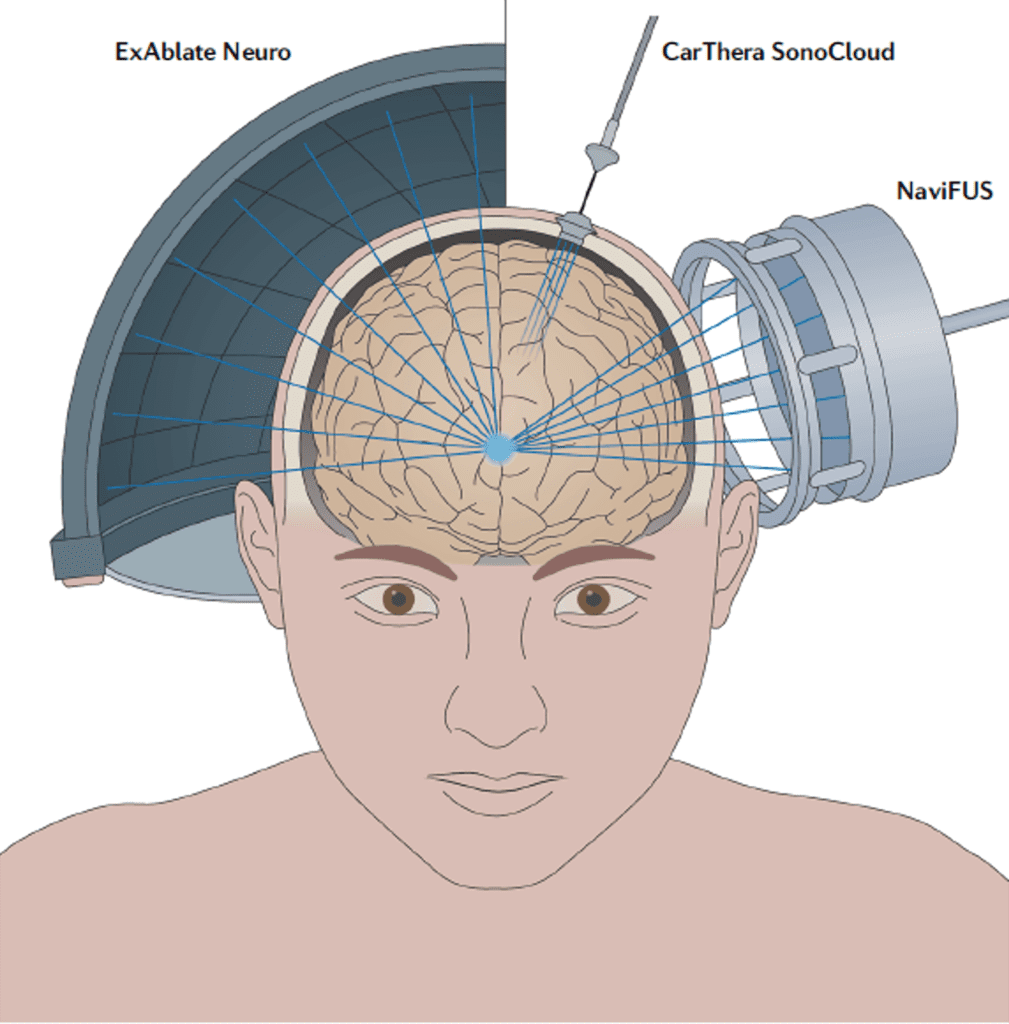
New hope is on the horizon for DIPG patients. A novel technique known as low intensity focused ultrasound, or FUS, is being used in the treatment of DIPG in conjunction with chemotherapy (Figure 2). By utilizing FUS, doctors can transiently and safely open space between the cells that line blood vessels in the brain (the BBB), thereby making it possible for drug molecules to move from the circulation and into tumor tissue. Other applications of FUS include generating heat to activate destruction of diseased tissue (hyperthermia and thermoablation), using sonodynamic therapy (SDT) to generate metabolites of a drug that are therapeutically active, and neuromodulation, which can be used to treat disorders like essential tremor.
There are several commercially available FUS devices available, each which delivers sonodynamic therapy with slightly different techniques (Figure 3). In some cases of this technology, doctors use FUS in combination with magnetic resonance imaging guidance (MRg) to help target the sonodynamic therapy to the correct anatomic location (Figure 4). This exciting new approach is being applied in several clinical trials in the US to treat pediatric brain tumors (clinicaltrials.gov). Here, we would like to highlight the two studies being done at Children’s National Medical Center in Washington DC with MR guided low intensity FUS in patients with DIPG.
The first clinical trial is known as SDT201. This is a dose-escalation study, examining the safety, pharmacokinetics, and preliminary efficacy of ascending drug and energy dose combinations for sonodynamic therapy using SONALA-001 (drug) in combination with Exablate 4000 Type-2 MR-Guided Focused Ultrasound (sonodynamic therapy device, Figure 4) in subjects with newly diagnosed DIPG. In this study, patients age 6 and older who have completed their standard of care radiation therapy and have stable (not progressive) disease are eligible to participate. A total of 18 patients will be enrolled and assigned to dose escalating cohorts. The drug under investigation in this study is SONALA-001 (aminolevulinic acid or ALA). Preclinical studies in mouse models of glioma have shown that sonodynamic therapy through MgFUS can activate protoporphyrin IX (PpIX), a metabolite of ALA, which in turn can cause glioma cell death (1-3). The team at Children’s National have reported their experience with the first patient of this study in the Journal of Neuro-Oncology (4).
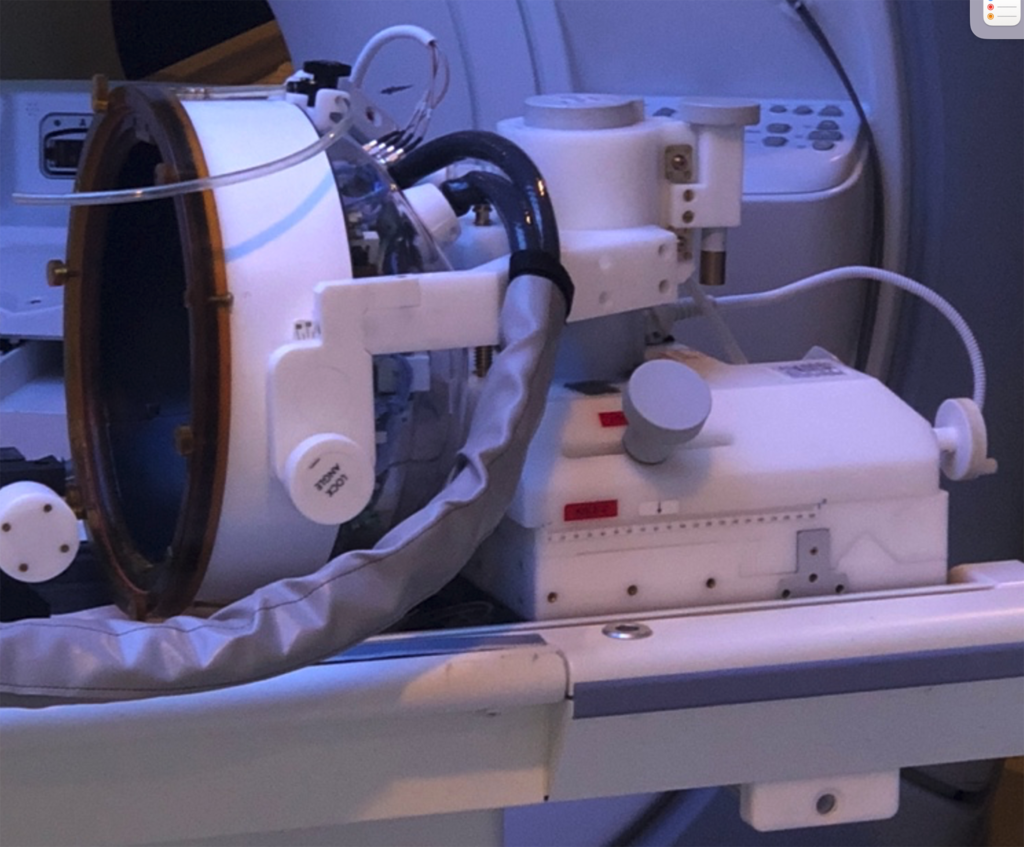
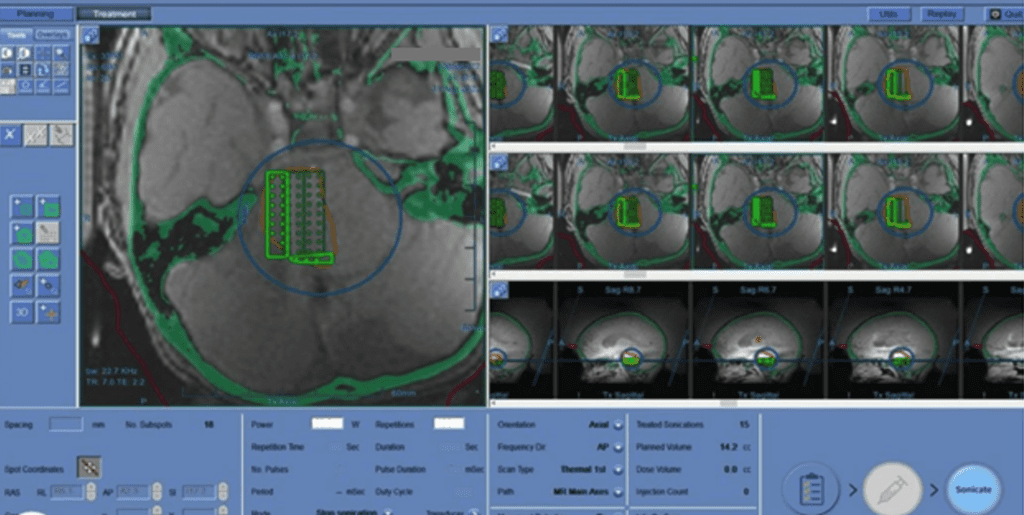
The second clinical trial is known as BT016. This is a safety and feasibility study to evaluate BBB disruption using Exablate MR-Guided FUS in combination with Doxorubicin (drug) in treating children with DIPG. In this study, children age 5 -21 with newly diagnosed DIPG and who have completed their standard of care radiation therapy and have stable (not progressive) disease are eligible to participate. Doxorubicin is thought to have an anti-tumor effect by disrupting tumor DNA structure and generating free radicals that damage tumor cells. Doxorubicin shows promising effects in mouse models of glioma and when delivered directly into tumor tissue, but is too toxic when delivered intravenously at doses adequate to cross the BBB. Therefore, using MRgFUS to open the BBB can help allow Doxorubicin to reach the tumor tissue, without the toxic side effects. In this study, MR imaging is performed to target the tumor with the sonodynamic therapy (Figure 5), and after the procedure to document BBB opening.
Dr. Hasan Syed, MD is Associate Professor of Neurological Surgery at the George Washington University, a pediatric neurosurgeon at Children’s National Medical Center, and the neurosurgical investigator of these studies. “Focused Ultrasound signals an innovative approach to treating children with DIPG. We are optimistic that continued research will enhance treatments and change the course of this disease.” Indeed, Dr. Syed and his team are giving new hope to patients and their families who are fighting this deadly disease.
References
- Jeong E-J, Seo S-J, Ahn Y-J, Choi K-H, Kim K-H, Kim J-K (2012) Sonodynamically induced antitumor effects of 5-aminolevulinic acid and fractionated ultrasound irradiation in an orthotopic rat glioma model. Ultrasound Med Biol 38(12):2143–2150. https://doi.org/10.1016/j.ultrasmedbio.2012.07.026
- Suehiro S, Ohnishi T, Yamashita D, Kohno S, Inoue A, Nishikawa M, Ohue S, Tanaka J, Kunieda T (2018) Enhancement of anti-tumor activity by using 5-ALA-mediated sonodynamic therapy to induce apoptosis in malignant gliomas: significance of high-intensity focused ultrasound on 5-ALA-SDT in a mouse glioma model. J Neurosurg 129(6):1416–1428.
- Wu S-K, Santos MA, Marcus SL, Hynynen K (2019) MR-guided focused Ultrasound facilitates Sonodynamic Therapy with 5-Aminolevulinic acid in a rat glioma model. Sci Rep 9(1):10465. https://doi.org/10.1038/s41598-019-46832-2
- Syed HR, Kilburn L, Fonseca A, Nazarian J, Oluigbo C, Myseros JS, Packer, RJ, Keating RF. First-in-human sonodynamic therapy with ALA for pediatric difuse intrinsic pontine glioma: a phase 1/2 study using low-intensity focused ultrasound. J Neurooncol. 2023 Apr;162(2):449-451. https://doi.org/10.1007/s11060-023-04269-8
Amanda Saratsis, MD
Board Member, Scientific Affairs
Jeri Wilson
Executive Director, CSPG