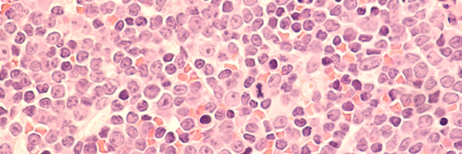
The hematologic (blood cell) malignancies persist as the most common cancer in children. However, many research advances have had a significant impact on clinical outcomes and survival in these patients. This is due in large part to innovative thinking and the collaborative nature of pediatric cancer research. One strong example is in childhood, adolescent and young adult non-Hodgkin Lymphoma (NHL), a disease area where PCRF has been a significant funder over the past 41 years. Progress over this time has led to >85-90% 2-year event free survival in many subtypes of childhood and adolescent NHL. The major subtypes of childhood and adolescent NHL include Burkett Lymphoma (BL), Diffuse Large B-Cell Lymphoma (DLBCL), Lymphoblastic Lymphoma (LL), and Anaplastic Large Cell Lymphoma (ALCL). These subtypes differ in terms of what cancerous blood cells arise, how they behave, and hence how they are treated.
Importantly, in October 2022, experts from around the world assembled in New York City and participated in the 7th International Symposium on Childhood, Adolescent and Young Adult NHL, chaired by Dr. Mitchell Cairo, MD and underwritten by PCRF. There, cutting edge research and expert clinical opinions were shared amongst attendees, resulting in the emergence of the “state of the science” for this disease. This month’s blog post focuses on some of these exciting advances and ongoing challenges in the diagnosis and treatment of childhood, adolescent, and young adult NHL, as also recently captured in the journal Best Practice & Research Clinical Haematology.
Targeted Immunotherapy for NHL
One important advance in NHL management is the use of targeted immunotherapy. Immunotherapy is effective in that it creates an environment where the body’s own immune cells specifically target and attack the cancer cells. This strategy includes the use of rituximab in mature B-Cell NHL, and brentuximab in ALCL, in combination with more standard chemotherapeutic drugs (a therapeutic approach hence termed chemoimmunotherapy). The use of targeted immunotherapy has resulted in a significant increase in event free survival (EFS) for these patients. In addition, it allows delivery of a decreased dose of chemotherapeutic agents or radiation therapy, reducing toxicity and significant side effects of these treatment modalities

Treating NHL in the Molecular Age
Another crucial advance in NHL diagnosis and treatment is the result of using next-generation sequencing technologies to study cancer specimens. This sequencing of DNA, RNA and even proteins in NHL has provided new insight into the molecular biology of the disease and its various subtypes. For example, researchers have learned that there are molecular aberrations in the NHL genome that result in cancerous cell growth and proliferation. Many of these aberrations occur in genes that encode for components of the immune system, lending further credence to an immunotherapy treatment approach for NHL. Indeed, as genetic sequencing data becomes more available and is shared by researchers, the more will be understood about this disease, which in turn will allow identification of novel therapeutic vulnerabilities that can be targeted for improved treatment.
Detecting Residual Disease
NHL is typically treated with rounds of chemotherapy followed by radiation, or with chemotherapy alone. Treatment may also include plasmapheresis and stem cell transplant, depending on the extent of disease and lymphoma subtype. After treatment, patients are monitored for residual disease, which is crucial to their clinical outcomes and determines what additional modalities of treatment may be necessary. Importantly, new techniques of minimal residual disease detection have been developed and tested in all major subtypes of childhood and adolescent NHL, including mature B-NHL, ALCL, and T-cell lymphoblastic lymphoma (T-LL). These tests have increased sensitivity and specificity for residual disease, making detection more likely if present. The most widely used tests include laboratory techniques known as flow cytometry, next-generation sequencing, and polymerase chain reaction. In each of these approaches, cancerous cells may be detected via their cell surface markers or their genomes. These tests can be performed on samples of bone marrow cells obtained via needle aspiration, and/or peripheral blood cells collected through a vein, making clinical application feasible
Ongoing challenges in NHL diagnosis and treatment
While these advances undoubtedly have improved outcomes in childhood, adolescent and young adult NHL, there are still challenges to disease detection and management, making room for opportunity to continue to push the boundaries of diagnostic and therapeutic approaches in this disease to improve further patient outcomes. Clinicians and researchers are now focused on several areas, such as investigating what treatment protocols will provide the best possible event free survival while minimizing toxicity and morbidity; determining the best possible treatment regimens for patients with relapsed or refractory disease; and increasing the use of sequencing technologies to improve our knowledge of the molecular biology of NHL to better understand disease transformation, progression and treatment resistance. Indeed, the collective goal of those who study and care for patients with childhood, adolescent and young adult NHL is to continue to improve survival, and even determine new methods of disease screening and prevention.
Amanda Saratsis, MD, Board Member, Scientific Affairs
Jeri Wilson, Executive Director, CSPG